Electronic Health Records (EHRs) are essential in healthcare, but for behavioral health providers, they often create more challenges than solutions. Poor usability leads to inefficiencies, clinician burnout, and reduced time for patient care. This article outlines actionable strategies to improve EHR systems for behavioral health professionals, including:
These improvements not only reduce administrative burdens but also enhance patient outcomes and clinician satisfaction.
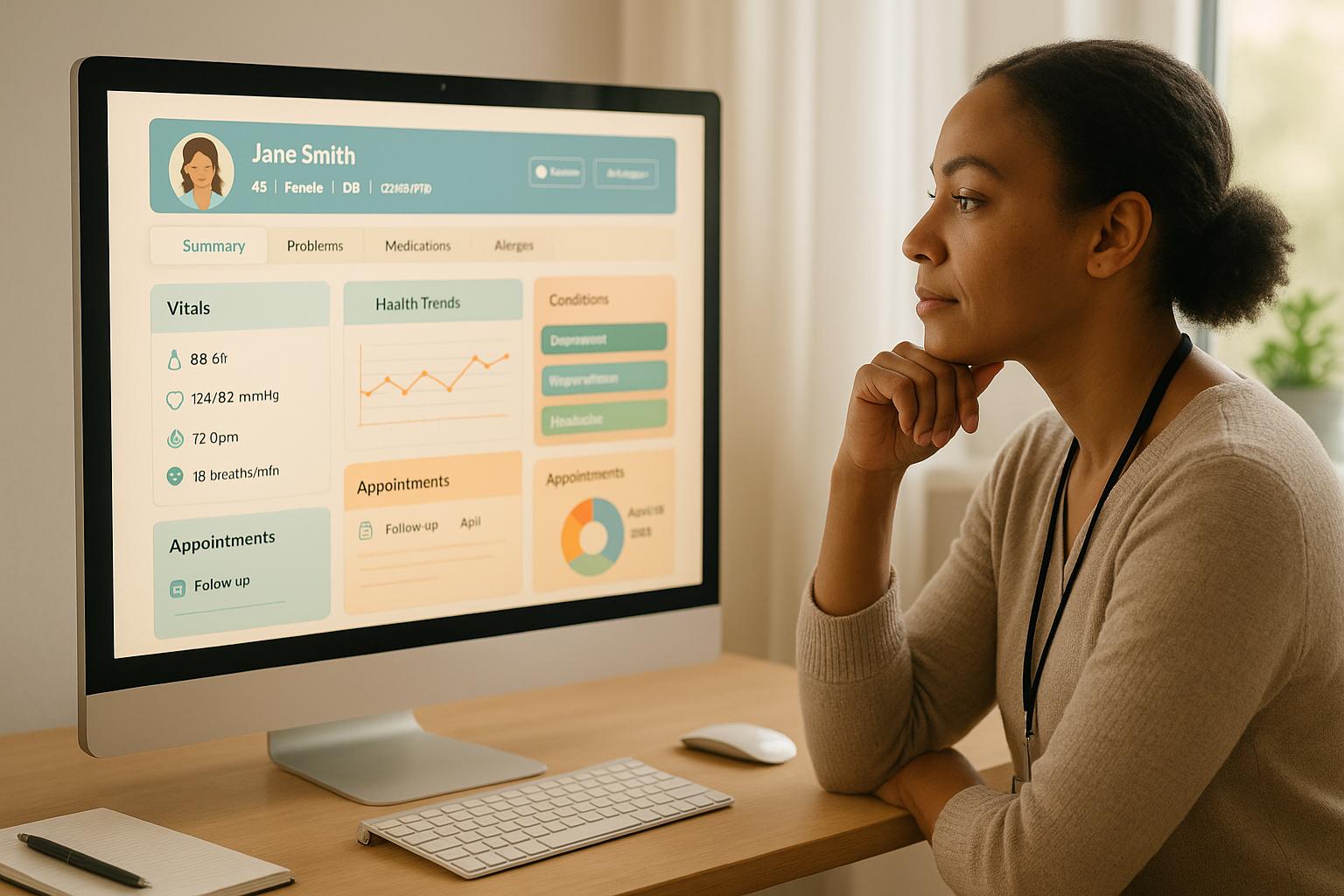
Designing an EHR system tailored for behavioral health professionals goes beyond just offering standard features. It’s about creating a tool that seamlessly fits into clinicians' workflows. When user experience is prioritized, daily tasks become smoother and more efficient.
"EHR usability in behavioral health directly impacts clinician productivity, patient engagement, and workflow efficiency."
Role-based dashboards are a game-changer for behavioral health EHRs. By customizing the interface to fit specific job roles, you eliminate the clutter of unnecessary options and make navigation far more intuitive. For instance, a therapist’s dashboard might highlight upcoming appointments, recent progress notes, and quick links to assessment tools. Meanwhile, a clinical supervisor’s view could focus on pending documentation, staff productivity metrics, and oversight tools. Administrative staff might see scheduling tools, insurance verification options, and billing updates front and center. This targeted approach ensures users spend less time clicking around and more time focusing on their tasks.
The benefits of such dashboards are clear. Companies that adopt tailored dashboards report a 5–6% boost in productivity, while visual productivity tools can slash project completion times by 30%. In healthcare, real-time dashboards have led to a 25% drop in diagnostic delays and a 30% reduction in diagnostic errors, particularly in high-pressure environments.
Beyond dashboards, intuitive navigation plays a vital role. By grouping related functions logically and keeping menu layouts consistent, users don’t have to waste time learning complex systems. Robust search tools further simplify workflows, allowing users to quickly find patients, documents, or features with just a few keystrokes. And when paired with customizable layouts, these tools make the system even more efficient.
Customizable interfaces take efficiency to the next level by letting clinicians tailor their screen layouts to match their specific needs. For example, custom templates can streamline documentation by pre-filling common fields, offering quick-select options for standard responses, and flagging required fields to ensure compliance. In behavioral health, these templates should align with DSM-5/ICD-10 criteria and include options for biopsychosocial assessments, progress notes, and discharge summaries.
Role-based access control (RBAC) adds another layer of efficiency and security. By restricting access to only the information and tools relevant to a user’s role, RBAC simplifies workflows while safeguarding sensitive patient data. This approach not only reduces administrative overhead but also strengthens data privacy measures.
Visual aids can also make a big impact. Studies show that visuals are processed 60,000 times faster than text, and decision-making improves by 28% when visualizations are used. Customizable dashboards that allow users to choose how data is presented - whether through charts, graphs, or other formats - can enhance understanding and speed up decision-making.
These customization capabilities lay the groundwork for mobile-first designs that ensure usability across all devices.
With more healthcare professionals relying on mobile devices to access EHRs, mobile-first design has become a necessity. A study at Penn Medicine highlighted the benefits of this approach. Their mobile app, Carelign, allowed teams to access real-time data 50% more often during rounds and cut login times by 25%. On mobile devices, logging into Carelign was 22 times faster than on desktop - 2.4 seconds compared to 52.8 seconds.
Mobile-first designs focus on touch-friendly interfaces and clear information hierarchies, making them ideal for smaller screens. Buttons and interactive areas should be at least 44×44 pixels to accommodate touch gestures. Essential data is displayed prominently, while less critical information is tucked into collapsible sections, ensuring users can quickly find what they need without feeling overwhelmed.
Multi-device access is another key feature, especially in behavioral health settings where care often happens outside traditional office environments. Whether clinicians are updating records from a tablet during a session or checking patient information from their phone on the go, consistent usability across devices ensures they stay connected and efficient. Prioritizing true mobile-first principles - rather than simply adapting desktop layouts - can significantly enhance user satisfaction and ultimately improve patient care.
Involving clinicians and staff in the development of electronic health record (EHR) systems is essential for creating tools that are both practical and effective in behavioral health settings. The success of an EHR implementation often hinges on input from all stakeholders - clinicians, support staff, and even patients. Without this input, organizations risk ending up with systems that might look good on paper but fail to meet the day-to-day needs of their teams, leading to frustration and inefficiency.
Behavioral health care presents unique challenges, with clinicians managing complex documentation, diverse treatment methods, and sensitive patient interactions. An EHR system designed without their input can quickly become an obstacle to quality care instead of a helpful tool.
Creating a functional EHR begins with assembling the right team. Forming an implementation committee that includes representatives from all key stakeholder groups ensures diverse perspectives are considered. This team might include therapists, psychiatrists, case managers, administrative staff, billing personnel, and IT support. Their first task should be identifying the features and functions the system needs to support their work. For instance:
Platforms like Lightning Step incorporate stakeholder input into their design, offering customizable reporting and AI-powered documentation tailored to real-world needs.
Getting this committee involved early is crucial. Early engagement allows time for gathering input, testing configurations, and refining the system based on feedback. Regular meetings - bi-weekly during planning and weekly as implementation nears - help keep the process on track. Once the design is drafted, usability tests and real-world feedback can validate its effectiveness.
Usability testing is more than asking users if they "like" the system. It involves observing how clinicians interact with the EHR during their daily tasks. A 2017 study highlighted the importance of methods like ethnographic observation and targeted questionnaires to identify usability issues.
Feedback should be collected throughout the process - before, during, and after implementation. Pre-implementation workflow analysis sessions, where staff demonstrate their current processes, can uncover pain points the new system should address while preserving what already works. Testing sessions should mimic real scenarios, such as therapists completing progress notes or billing staff processing claims. Observing where users struggle or hesitate can reveal potential problems that might not surface during formal training.
Establishing regular feedback loops is essential. Weekly check-ins during testing phases can catch issues early, while monthly surveys after the system goes live can track satisfaction and flag new concerns. Offering anonymous feedback options encourages honesty, helping to identify limitations or training gaps.
Even after the system is live, ongoing staff input is vital for continuous improvement. Behavioral health organizations, in particular, must prioritize feedback to ensure the EHR remains safe and user-friendly, as documentation errors can directly impact patient care.
Training programs should include "super-users" who act as advocates for the system. These individuals serve as a bridge between everyday users and system administrators, collecting feedback and troubleshooting common issues. Super-users often identify practical workflow enhancements, like custom templates or alert configurations, that may not have been apparent during initial implementation.
Real-world examples show the value of this approach. Praesum Healthcare reported that their EHR evolved into an essential resource for clinicians, improving documentation efficiency and overall facility performance. Similarly, Woodlake Recovery Center noted that their system helped reduce burnout and improve patient outcomes.
Behavioral health settings, where medication interactions and crisis situations demand careful documentation, particularly benefit from systematic feedback collection. Regular tools like Safety Culture surveys or monthly pulse surveys can track user satisfaction, while quarterly focus groups provide deeper insights into potential system improvements. Using tools like the Hospital SOPS and Health IT item set before and after system updates can help evaluate the impact of changes.
As the American Medical Association warns, "burdensome EHR systems are a leading contributing factor in the physician burnout crisis and demand urgent action". Adhering to best practices in EHR design and feedback collection can minimize these risks and improve outcomes for both clinicians and patients.
Lightning Step's integrated platform offers a solution to many of these challenges by combining EHR/EMR, CRM, and RCM tools in one system. This reduces the need to switch between multiple platforms while allowing for customization based on ongoing feedback. Features like telehealth, medication management, and referral tools can be tailored to meet evolving organizational needs, ensuring the system grows alongside its users.
In behavioral health, administrative tasks take up nearly double the time spent on patient care. This imbalance not only exhausts clinicians but also limits the time they can dedicate to their patients. Automation and artificial intelligence (AI) present practical solutions to shift this balance, enabling organizations to simplify workflows and prioritize patient care.
A study revealed that 78% of physicians reported better patient care after adopting electronic health records (EHRs). Moreover, automated scheduling and reminders have been shown to reduce missed appointments by up to 23%.
Automation excels at handling repetitive tasks like appointment reminders, prescription refills, billing, and documentation. By automating these processes, organizations can reduce manual errors and free up staff to focus on more complex patient care.
The success of automation depends on selecting the right tasks. Processes that involve manual data entry, frequent repetition, and clearly defined variables are ideal candidates. For example, automated appointment reminders help cut down on no-shows, while standardized templates streamline routine documentation.
| Good Candidates for Automation | Challenges for Automation |
|---|---|
| Manual data entry | Tasks requiring complex, inconsistent decision-making |
| High-frequency tasks | Processes with unpredictable data requirements |
| Clearly defined variables | Decision-making influenced by unclear variables |
| Clear roles and responsibilities | Undefined roles or inconsistent workflows |
When EHR systems integrate seamlessly with lab systems, billing software, and scheduling tools, data can flow between platforms without manual input. This reduces transcription errors and eliminates duplicate data entry.
Behavioral health organizations should focus on automating tasks like intake and risk assessments, medication tracking, and billing. These areas typically involve high-volume, routine work, making them well-suited for automation while ensuring compliance with HIPAA regulations.
This streamlined approach creates a foundation for AI tools to further ease documentation burdens.
Clinical documentation is one of the most time-intensive aspects of behavioral health, with clinicians spending 34% to 55% of their workday on EHR notes. This translates to an annual opportunity cost of $90 to $140 billion in the U.S.. AI-powered tools can significantly reduce this workload while maintaining accuracy.
AI enhances documentation by structuring free-text data, annotating notes, evaluating their quality, identifying trends, and flagging errors before they affect patient care. This combines the flexibility of free-text with the efficiency of structured data.
For instance, AI-driven speech recognition can cut documentation time by 19%–92%. However, success depends on proper implementation and clinician training.
Real-world examples highlight AI’s potential. Kintsugi, an AI-powered teletherapy platform, uses facial and voice analysis to provide therapists with real-time emotional insights during sessions. This not only improves documentation accuracy but also enhances therapeutic outcomes.
AI can also act as an assistant during patient encounters by recording audio, supporting clinical decisions, calculating risk scores, and suggesting clinical codes. While reducing the cognitive load on clinicians, it ensures comprehensive and precise documentation.
However, AI tools require careful oversight. Current systems detect 67% of sentence-level edits and 45% of word-level edits, emphasizing the need for human review. By reducing errors and the time spent on documentation, AI helps combat the inefficiencies contributing to clinician burnout.
For automation to be effective, EHR systems must integrate smoothly into existing workflows. Organizations should assess their clinical documentation, scheduling, billing, and administrative tasks to identify areas where integration could have the most impact.
Lightning Step offers a great example of integration by combining EHR/EMR, CRM, and RCM tools into a single platform. This eliminates the need for switching between multiple systems while providing AI-powered documentation, telehealth features, medication management, and custom reporting. Its automation tools handle routine tasks like scheduling, billing, and documentation templates.
When selecting automation tools, it’s essential to choose systems that can easily integrate into existing digital ecosystems, regardless of the organization’s size or technological capabilities. The aim is to simplify workflows and reduce reliance on paper forms and redundant data entry.
Seamless integration ensures automation works in harmony with existing systems. Engaging staff early in the process, providing thorough training, and offering ongoing support are key to ensuring a smooth transition. Establishing clear protocols to monitor and adjust automation based on real-world use is equally important.
The most successful implementations connect clinician and patient workflows, creating a system where information and care align seamlessly. By thoughtfully adopting automation and AI, behavioral health organizations can reduce administrative loads, improve documentation, and dedicate more time to patient care. This approach not only simplifies operations but also addresses burnout and enhances outcomes.
For electronic health record (EHR) systems to truly enhance patient care, they need to integrate seamlessly with tools like billing software, pharmacy networks, referral systems, and other related platforms. This interconnectedness allows organizations to break down silos, minimize redundant tasks, and provide more coordinated, efficient care.
A unified patient record depends on EHR systems that can effectively communicate with the various platforms an organization uses. This often means linking practice management systems, billing tools, pharmacy databases, and external referral systems to create a smooth flow of information.
Take, for example, a private therapy group in Austin, Texas. By integrating their EHR with their practice management system, they managed to cut administrative time by 40% and reduce claim rejections by 30%. Achieving results like these starts with evaluating current systems, setting clear goals for integration, collaborating with IT experts or vendors, and ensuring thorough testing and staff training. When direct integration between systems isn’t possible, third-party automation platforms like Zapier or Make.com can step in to handle tasks like appointment reminders and form submissions.
Key integration features include secure data sharing, customizable workflows, and advanced reporting tools. These ensure patient information remains protected while moving efficiently through the organization. Additionally, this streamlined data sharing enables systems to deliver precise, role-specific alerts.
Integrated EHR systems are powerful tools for improving patient safety and outcomes, thanks to real-time alerts and clinical decision support. These systems can flag potential medication interactions, remind clinicians about overdue assessments, and issue risk-based alerts for patients who need immediate attention.
Customizing alerts for specific roles can significantly improve workflow. For instance, prescribers might get notifications about possible medication conflicts, while case managers could receive updates on missed appointments or pending insurance authorizations. However, finding the right balance is essential - alerts must be helpful without overwhelming staff and causing alert fatigue. By accessing a complete view of a patient’s care, including medication history and billing details, EHR systems can provide the context clinicians need to make informed decisions. Platforms like Lightning Step are designed to excel in this area.
Lightning Step offers an all-in-one solution by combining EHR/EMR, CRM, and RCM tools into a single platform. This eliminates the need to juggle multiple systems, streamlining workflows and reducing potential data-sharing hurdles.
The platform also integrates with popular third-party tools like Twilio, Salesforce, Waystar, and CallTrackingMetrics. This flexibility allows organizations to continue using their preferred tools while benefiting from centralized data management. Additionally, Lightning Step provides built-in e-prescribing features, removing the need for external platforms like Dr. First.
The results speak for themselves. Organizations using Lightning Step report saving over 12.5 hours per month on documentation tasks, thanks to AI-powered tools. This not only boosts efficiency but also enhances revenue cycle management. By consolidating multiple functions, Lightning Step reduces administrative workloads and improves care coordination, aligning perfectly with the goal of empowering clinicians to focus on patient care.
"We chose Lightning Step because they are knowledgeable in our industry. Their services help streamline our documentation processes, increase authorizations for clients, increase revenue through billing, and our overall follow-up processes."
"Lightning Step brought a consolidated approach for both our Clinical and Revenue Cycle processes."
Lightning Step holds a 4.5 out of 5 rating on Software Advice, with strong marks for ease of use (4.3), value for money (4.4), and functionality (4.4). Users frequently highlight the platform’s intuitive design and responsive customer support, though some note room for improvement in mobile app functionality. With EHR adoption in behavioral health growing by nearly 45% since 2009, Lightning Step’s unified approach helps organizations simplify vendor management while ensuring seamless data sharing across all areas of patient care.
Once workflows are streamlined and systems are integrated, the next step is ensuring users are properly trained and supported. Even the most advanced EHR system won't succeed if users aren't equipped to utilize it effectively. A study found that 43% of users rated their initial EHR training as "less than adequate", and 94.6% believed their skills in using EMR systems could be improved. This disconnect between the system's potential and the user's ability to operate it can directly affect patient care and staff satisfaction, particularly in behavioral health settings.
EHR training works best when it acknowledges the unique responsibilities and technical skills of each role. For instance, a psychiatrist prescribing medications requires a different level of expertise compared to a front desk coordinator handling appointment scheduling or a case manager managing treatment plans. Role-specific training ensures that each team member focuses on the tools and workflows most relevant to their daily tasks.
Administrative staff, for example, will benefit from mastering appointment scheduling, insurance verification, and billing procedures. Clinical staff, on the other hand, need to become proficient in documentation templates, treatment planning tools, and medication management features.
Assessing each individual’s computer literacy is a crucial first step. Some team members may need basic computer training before diving into EHR-specific skills, while others may be ready to explore advanced functionalities right away. Setting SMART goals - specific, measurable, achievable, relevant, and time-bound - helps structure the training process and keeps progress on track. A mix of hands-on practice, online tutorials, and group discussions can accommodate different learning preferences.
Onboarding new employees is a critical moment for EHR adoption. Start with pre-boarding tasks like verifying credentials and setting up role-based system access. During the onboarding process, gradually introduce responsibilities under close supervision. For example, new clinical staff might begin by shadowing experienced colleagues before entering data themselves, while administrative staff can start with basic tasks like scheduling before moving on to more complex workflows.
Having "super users" within each department can make a significant difference. These individuals, who are highly trained in the system, act as peer mentors. In one organization, super users were temporarily relieved of their regular duties during the first week of implementation to focus solely on training their coworkers on billing, documentation, and navigation.
As EHR systems are updated with new features, refresher training becomes essential. Regular training sessions, combined with milestone assessments at 30, 60, and 90 days, help identify knowledge gaps and ensure staff remain confident in using the system.
Initial training is just the beginning - ongoing support is essential to help users stay proficient, adopt updates, and minimize errors. Combining internal expertise with vendor resources often yields the best results. Internal super users can provide immediate, context-specific assistance, but they need adequate time and resources to do so effectively. Regular feedback sessions offer a chance to address challenges, share tips, and gather suggestions for system improvements.
Creating a culture of continuous learning, where achievements are recognized and celebrated, can keep staff motivated and help identify future champions for system optimization.
Lightning Step simplifies this process by offering a unified platform that combines EHR, billing, and practice management tools. This integrated approach reduces the complexity of training on multiple systems, allowing staff to focus on mastering one cohesive solution that aligns with the streamlined workflows discussed throughout this guide.
Improving EHR usability in behavioral health requires addressing both technical design and human factors. Research shows clinicians spend a significant amount of their workday navigating EHR systems, which underscores the importance of making thoughtful, strategic improvements.
A user-centered design approach is critical for creating effective EHR systems. Features like role-based dashboards, customizable screen layouts, and mobile-friendly interfaces help reduce mental strain and prevent workflow interruptions - key contributors to clinician burnout. Since poor usability is a major driver of burnout, optimizing these systems has become an urgent focus.
In addition to user-centered design, involving stakeholders during the development process is essential. Input from clinicians, administrative staff, and other team members ensures the system aligns with real-world workflows. This collaborative approach helps identify potential issues early, avoiding costly setbacks.
Efficiency gains also rely on smart use of technology. Automation tools and AI integrations can save time and reduce manual tasks. For example, mental health facilities using AI-powered documentation tools report saving over 12 hours of paperwork per provider each month. Similarly, mid-sized addiction treatment centers with integrated CRM/EMR systems have seen a 65% reduction in admissions processing time.
Smooth data sharing further enhances workflows. System integration combats data fragmentation, a common challenge in behavioral health. Networks that adopt specialized billing software have reported clean claim rates increasing from 75% to 93%, along with a 40% drop in days spent in accounts receivable.
Beyond system design and integration, effective training is crucial. With 96% of U.S. hospitals now using EHR systems, organizations that provide ongoing, role-specific training see higher adoption rates and greater user satisfaction. Moving away from one-time training sessions and fostering a culture of continuous learning ensures these improvements stick.
Lightning Step, for instance, combines EHR, CRM, and RCM functions to simplify workflows for behavioral health organizations. A client from Into Action Recovery Center shared:
"We chose Lightning Step because they are knowledgeable in our industry. Their services help streamline our documentation processes, increase authorizations for clients, increase revenue through billing, and improve our overall follow-up processes."
To make sure an EHR system truly supports the needs of clinicians and staff, it’s crucial to involve them at every stage of the design and implementation process. This means collecting their feedback early on, integrating their suggestions into workflows, and tailoring features to fit their daily responsibilities. Offering consistent training and giving staff the chance to test the system before it goes live can also boost confidence and ensure the platform aligns seamlessly with clinical practices.
Take Lightning Step, for example. This platform stands out by providing customizable, all-in-one solutions that simplify everything from admissions to billing. By focusing on user feedback and adapting workflows, Lightning Step not only helps reduce staff burnout but also increases efficiency and enhances patient care. It’s a strong option for behavioral health organizations looking for a system that truly works for their teams.
Integrating AI and automation into EHR systems is reshaping how behavioral health organizations operate. AI brings sharper diagnostic capabilities, helps craft personalized treatment plans, and identifies mental health issues early, paving the way for improved patient care. On the other hand, automation takes over repetitive tasks like scheduling, clinical documentation, and billing, cutting down on administrative work so clinicians can devote more time to their patients.
This powerful combination boosts efficiency, reduces errors, and elevates the quality of care provided. Platforms such as Lightning Step take things a step further by merging EHR/EMR, CRM, and RCM tools into a single, user-friendly system. With features like AI-driven documentation, telehealth integration, and customizable reporting, Lightning Step enables behavioral health organizations to streamline their processes, ease staff workloads, and focus on delivering patient-centered care with greater efficiency.
To make EHR training and support effective in behavioral health settings, it’s important to start by evaluating your staff's technical abilities and customizing the training to meet their needs. Providing hands-on practice in simulated environments and offering step-by-step, process-focused guidance can help new users get comfortable with the system more quickly. One helpful approach is designating superusers - team members who are deeply trained in the EHR system. These individuals can act as go-to resources, offering peer support and building confidence within the team.
For long-term success, ongoing education is key. Regular refresher sessions and updates on new features can keep users engaged and operating efficiently. Platforms like Lightning Step streamline training and support with their user-friendly design and built-in tools, making it easier for organizations to onboard staff and maintain high levels of proficiency compared to other systems.



